Originally published by WBUR/CommonHealth on June 18, 2019. Written by Colin A. Young, State House News Service.
At a time when consumers are paying more attention to nutrition and the source of their food, the state could do more to integrate food into health care as a way to address chronic conditions and avoid some health care spending, a new report found.
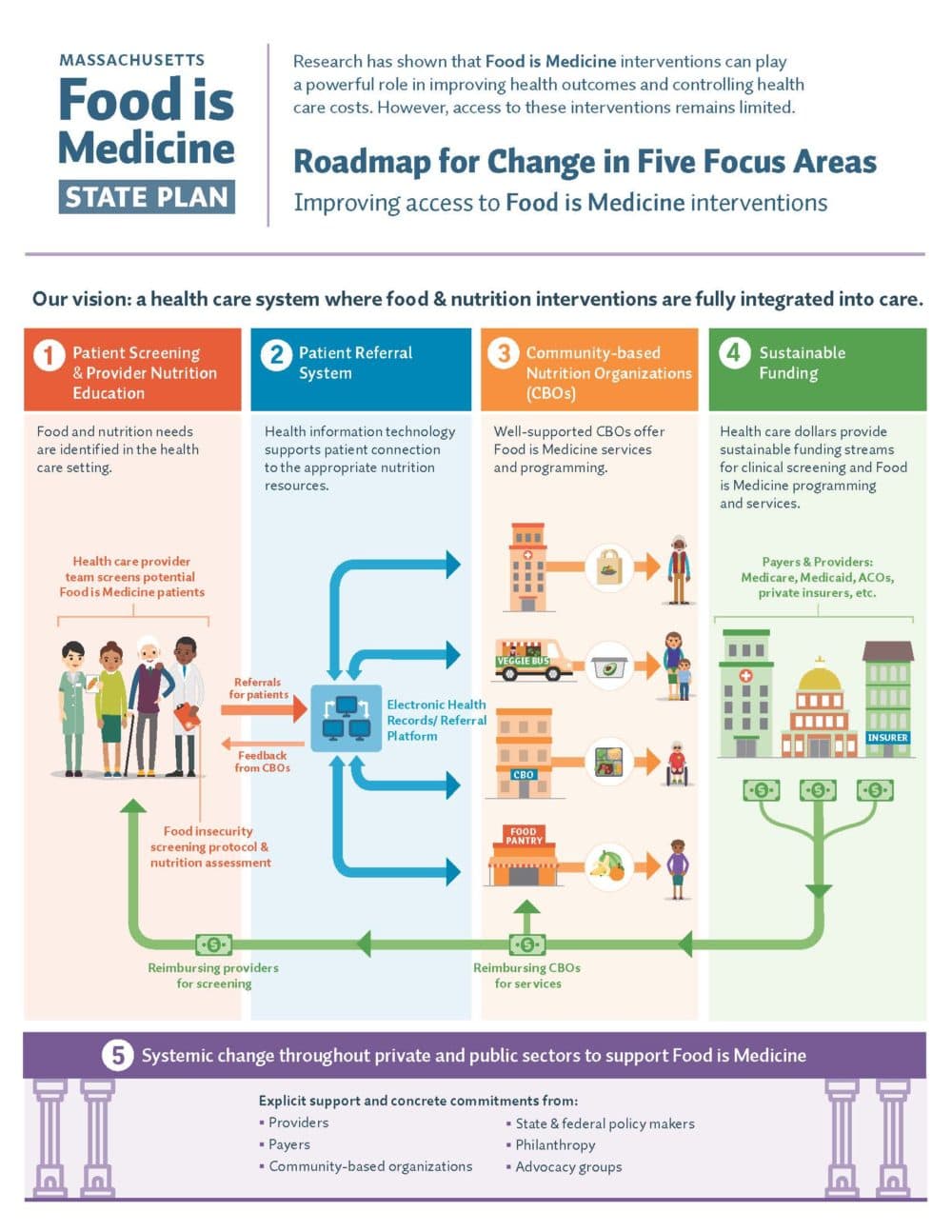
The Food is Medicine State Plan, a joint effort of the Center for Health Law and Policy Innovation of Harvard Law School and service provider Community Servings, focused on nutrition’s link to chronic diseases like diabetes or cardiovascular disease, and the notion that food can act as medicine when meals are tailored to meet the specific needs of people living with or at risk for certain serious health conditions.
The report was released Tuesday at an event featuring Sen. Julian Cyr and Rep. Denise Garlick.
About one in 10 households in Massachusetts struggles with food insecurity, or not having consistent access to enough food for a healthy and active lifestyle, leading to $1.9 billion in annual health care costs that could be avoided, the report said.
Though Massachusetts has programs that try to address the issue of food insecurity and inaccessibility of fresh foods, the report said access to food as medicine programs remains limited in the state and across the country. But as consumers think more about the food they eat, and as Massachusetts shifts its Medicaid program into an Accountable Care Organization model, the report says the time is now to integrate food and medicine.
“We can build a system that reliably identifies individuals who are food insecure, connects them to appropriate Food is Medicine interventions, and supports those interventions via sustainable funding,” the report concluded. “In doing so, Massachusetts will establish itself as the first state in the nation to ensure that patients have access not only to affordable, effective medical care but also to the foods they need to live healthy, happy and productive lives.”
The report said there are 736 food pantries, meal programs, food rescue organizations and produce voucher programs in Massachusetts, but only 63 of them work with health care providers or tailor meals to meet specific medical needs.
The new ACO system, the report said, provides a ripe opportunity to integrate food is medicine policies because program requirements and financial incentives are changing to leverage community-based resources.
“For example, MassHealth will require ACOs to screen patients for health-related social needs, including food insecurity,” the report said. “Starting in January 2020, ACOs will also receive Flexible Services funding that can be used to provide access to services that respond to health-related social needs, including Food is Medicine interventions.”
The report’s authors recommend that professional medical societies and providers work together to increase provider nutrition education and referral capacity, that MassHealth issue guidance on food insecurity and malnutrition screening protocols, and that insurers incentivize provider networks to screen for food insecurity and make resource referrals part of patient care.
The Legislature should “explicitly recognize Food is Medicine as a priority through legislative action and within the state budget” by funding a pilot program to evaluate the impact of Food is Medicine within the MassHealth population, providing enough funding to meet the demand of the Healthy Incentives Program and by funding the Prevention and Wellness Trust Fund.
To build on the report, its organizers in the coming months plan to convene three task forces within the Massachusetts Food is Medicine Coalition to focus on strategies to address some of the issues identified in the report.
One task force will look at ways to improve the capacity of health professionals to identify and address the need for food is medicine interventions in patients. Another will “lead a statewide effort to establish standards for Food is Medicine interventions in the Commonwealth” and the third will develop research plans to advance the public health and medical understanding of food insecurity and food is medicine programs.


Food Law & Policy, Commentary
Policy to Reduce Methane Emissions and Feed More People
April 3, 2025